Understanding Inflammation: How to Heal Smarter, Not Just Harder
A physical therapist’s guide to calming inflammation and improving recovery
✅ 1. Introduction: Why This Matters
“You’ve probably been told your pain or swelling is just inflammation, but what does that really mean?”
Inflammation is often misunderstood, but it’s one of your body’s most powerful tools for healing. If you’ve ever experienced pain, swelling, or surgery, understanding inflammation is key to smarter recovery.
Inflammation isn’t the bad guy. In fact, it’s one of your body’s most vital tools for healing and protection. But like any tool, when it’s misused or unchecked, it can do more harm than good.
Whether you’re recovering from a sprain, managing post-op swelling, or dealing with long-term joint pain, this article will help you understand:
What inflammation actually is (and isn’t)
Why it lingers longer than it should
How you can reduce it naturally without stopping the healing process
2. What Is Inflammation, Really?
Inflammation is your body’s built-in alarm and repair system.
When tissue is damaged, whether from a rolled ankle, surgical incision, or repetitive stress, your immune system sends out signals to increase blood flow, deliver healing cells, and kickstart repair.
It’s like a construction crew arriving after a storm: they bring tools, materials, and reinforcements, but they also make noise, block traffic, and create a mess while working.
“Something happened here—let’s fix it.”
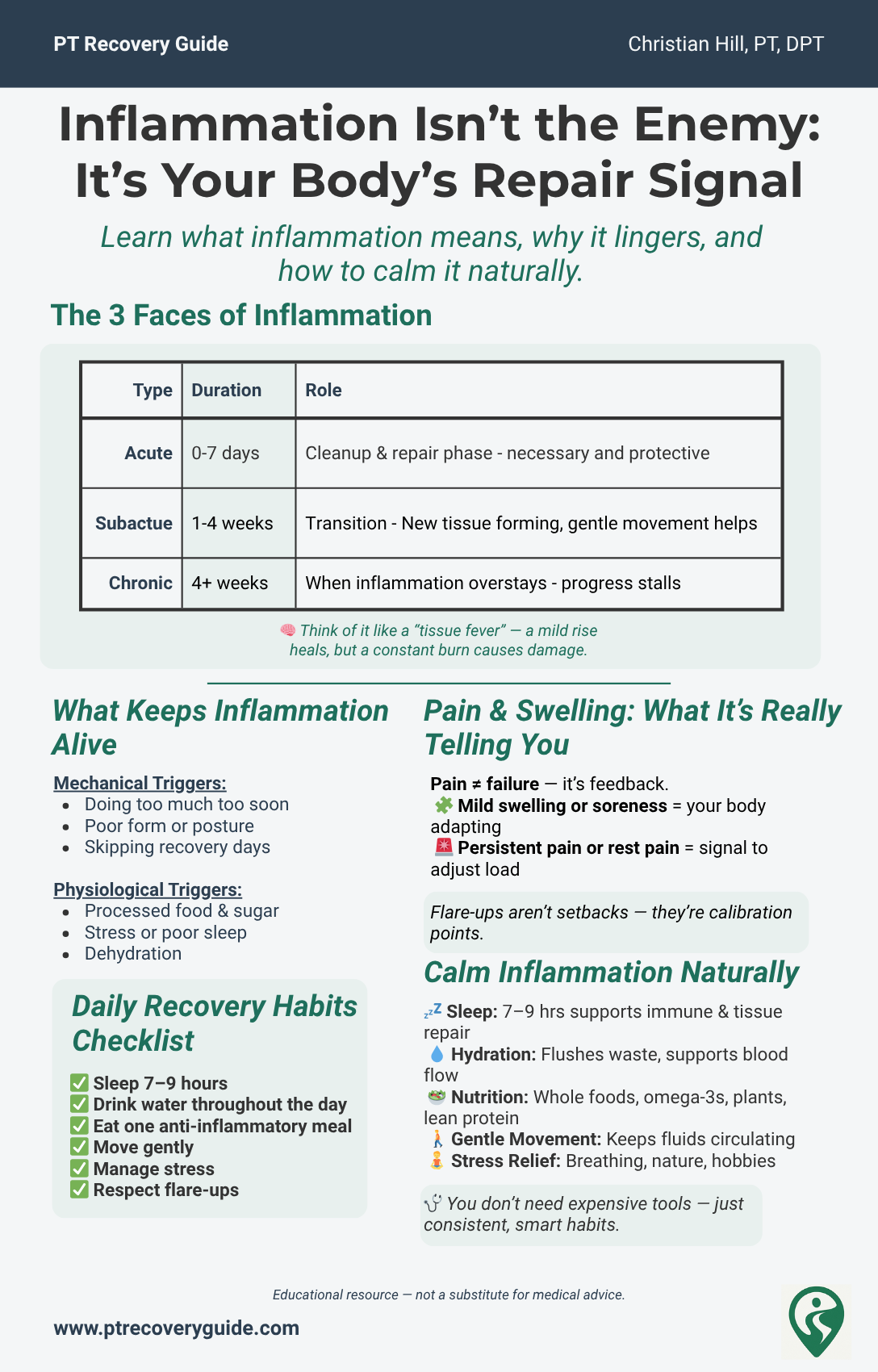
Two Types of Inflammation:
Acute Inflammation This is the short-term, healthy version. It creates warmth, redness, swelling, and pain—all part of the healing process. It typically resolves in a few days to a couple weeks if properly supported.
Chronic Inflammation This occurs when the “clean-up crew” overstays its welcome. The immune response doesn’t turn off, either due to repeated irritation or systemic dysfunction. Chronic inflammation can actually break down tissue over time, delay healing, and heighten pain sensitivity.
🌡️ Think About It
Think of inflammation like a tissue fever — a mild elevation is helpful, but a persistent spike can become dangerous.
Or like a sprinkler system — it’s lifesaving in a fire, but damaging if it keeps spraying long after the fire’s out.
3. How Inflammation Affects Healing Over Time
Knowing which stage of healing you're in helps you choose the right strategies. Here's a simplified timeline:
| Phase | What’s Happening | What You Might Feel | Why It Matters |
|---|---|---|---|
| Acute (0–7 days) | Immune cells rush in to clean up debris and protect tissue | Swelling, heat, stiffness, pain | Critical for setting the stage for repair |
| Subacute (1–4 weeks) | Tissue rebuild begins; inflammation tapers | Soreness, occasional stiffness | Gentle movement supports collagen remodeling |
| Chronic (4+ weeks) | Lingering low-grade inflammation or poor tissue adaptation | Achiness, tightness, plateaus | Healing stalls or regresses without smart rehab |
👉 Supporting your body through inflammation, not by avoiding it completely, is key to smarter, faster recovery.
4. Common Inflammation Triggers During Rehabilitation
If your swelling or pain just won’t go away, the problem may not be the injury anymore, it could be the habits keeping the inflammation alive.
🔧 Mechanical Triggers (External)
Doing too much too soon
Improper form or posture during exercise
Skipping recovery days
Repetitive strain without variation or support
🔬 Physiological Triggers (Internal)
Highly processed diet (sugar, seed oils, alcohol, etc.)
Dehydration (even mild dehydration affects cellular healing)
Emotional stress (increases cortisol, which is pro-inflammatory)
Poor sleep (1 night of sleep deprivation can spike inflammatory cytokines)
These factors raise your body’s “inflammatory threshold,” making you more sensitive to activity and more prone to flare-ups—even from small tasks.
5. How to Calm Inflammation Naturally
You don’t need expensive gadgets, injections, or pills to improve inflammation. Some of the best evidenced based tools are free, modifiable, and lifestyle based.
| Tool | Why It Works | PT Tips |
|---|---|---|
| ✅ Sleep | Deep sleep supports immune regulation and collagen repair | 7–9 hours/night. Prioritize consistency. |
| 💧 Hydration | Aids waste removal and improves blood flow | Aim for ½ bodyweight in ounces (more if sweating) |
| 🥗 Anti-inflammatory Nutrition | Nutrients like omega-3s, fiber, and antioxidants reduce systemic inflammation | Focus on colorful plants, fatty fish, nuts/seeds, and lean protein |
| 🚶 Gentle Movement | Helps drain lymphatic fluid, prevents stiffness, maintains blood flow | Try ankle pumps, light walking, mobility circuits |
| 🧘 Stress Reduction | Cortisol drives inflammation when chronically elevated | Use breathwork, nature, creative hobbies, or music |
6. Progress Isn’t Linear, But Inflammation is a Clue
Inflammation acts like a check engine light, not a stop sign.
Instead of seeing pain or swelling as failure, see it as feedback. Your body is telling you something needs adjusting.
🚩 Clues to Watch For:
Local swelling/redness that increases after activity
Pain lingers for longer than expected after exacerbation
Pain while at rest
Throbbing or difficulty sleeping due to activities earlier
Use these signs to guide:
Activity pacing (how much and how often)
Exercise choices (what your tissue can handle)
Recovery needs (when to rest, ice, hydrate, sleep)
⚡ Pro Tip: Flare-ups aren’t failures. They’re calibration moments, a chance to reset and realign.
How to Respond:
When inflammation has increased, it is important to give yourself permission to take a break and address it. Pushing through painful inflammation and further irritating inflammed tissues may only exacerbate it.
Allow for some intentional rest (with elevation)
Gentle, non-painful massage of the area in strokes that lead back to the trunk
Compression using bandages or compression garments
Medicinal management if cleared or recommended by physicians (NSAIDs, etc.)
Dialing down/back the frequency, duration, or intensity of aggravating activites in the short-term.
It is important to not completely discontinue from the rehabilitation process if inflammation is occurring, it is a natural process, and will likely be present. It just important to moderate the extent to which it is pushed and at what level it is allowed to occur.
👉 Want more information regarding how to use ice vs heat? Check out our article: Ice vs Heat for Injury: A Physical Therapist’s Guide to Pain & Swelling Relief
7. Quick Checklist: Daily Inflammation Habits
| ✅ Habit | Daily Goal |
|---|---|
| Sleep 7–9 hours | Protects healing and hormone balance |
| Drink water throughout the day | Improves cell function and tissue flush |
| Eat one anti-inflammatory meal | Prioritize whole foods and plants |
| Move gently | Walk, stretch, or mobility flows |
| Manage stress | Breathing, rest, sunlight, or laughter |
| Respect flare-ups | Don’t ignore—adapt and recover |
⚡Tip: For a week-by-week breakdown of post-surgical inflammation for knee replacements, see our total knee replacement recovery guide
Closing Thoughts: Understanding Builds Confidence
Inflammation isn’t the enemy—it’s information.
If you learn to listen to it and support it, you gain control over your recovery. You don’t need to be perfect to heal—you just need to stay curious, consistent, and compassionate with your body.
Whether you’re managing post-op pain, returning from injury, or dealing with chronic inflammation, the principles are the same:
Move intelligently
Rest purposefully
Support your system from the inside out
Eat to Heal, Not Just to Recover
Inflammation starts in the body—but what you eat can help control it.
Download the Anti-Inflammatory Eating Starter Guide and Daily Checklist, built by a physical therapist to help you reduce pain, support healing, and feel better every day.
Simple, evidence-based steps. No diets. No fluff.
References:
Medzhitov, R. Origin and physiological roles of inflammation. Nature 454, 428–435 (2008). https://doi.org/10.1038/nature07201
Irwin MR. Why sleep is important for health: a psychoneuroimmunology perspective. Annu Rev Psychol. 2015;66:143-172. doi:10.1146/annurev-psych-010213-115205
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377. doi:10.1126/science.1241224
Calder PC. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans. 2017;45(5):1105-1115. doi:10.1042/BST20160474
Rohleder N. Stimulation of systemic low-grade inflammation by psychosocial stress. Psychosom Med. 2014;76(3):181-189. doi:10.1097/PSY.0000000000000049
Written by Christian Hill, PT, DPT, CDNT – Licensed Physical Therapist with over 10 years in orthopedic rehab.
This article is for educational purposes only and is not a substitute for professional medical advice. Always consult with your healthcare provider before beginning any new rehabilitation or treatment plan.
Updated: 10/21/2025